Image by quinn.anya
It's great to see the growth of discussion in medical education on Twitter. Recently I have seen a few really interesting cases being discussed (and a lot being learned), but there have also been some questions about how we together can think about what is best practice in leading these discussions.
Case discussions have always been a very important way of learning in medicine. And as one doctor said, junior staff are still encouraged to submit cases to journals, but it can take many months for a case submitted to a journal to reach publication. In the meantime, social media removes those barriers to publication. We can all self-publish. But we have to be responsible too. I think that all of the people currently involved in leading discussions are being responsible, but how do we make clear to others what best practices we are following? I think that it is important to consider this for a few reasons. First, we have an obligation to all patients to make these discussions safe. Second, we are modelling how to share these cases to other students and professionals.
We also need to think about whether the existing guidance, which in the UK is from the GMC, is sufficient to guide us.
So a few questions....
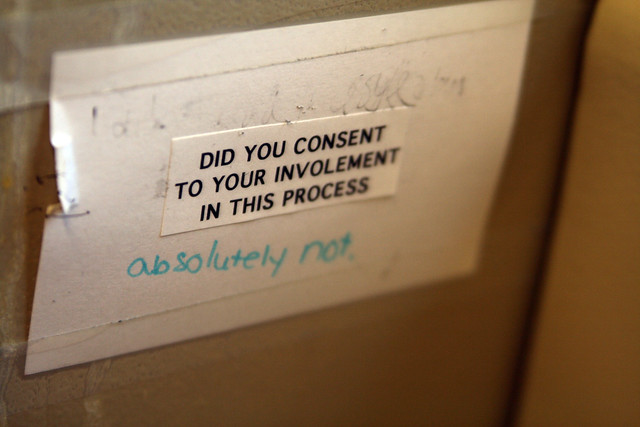
What should we tell patients about sharing their story? Do we need their consent if the story is not recognisable to others?
When the GMC discuss confidentiality the emphasis is on not sharing information (without consent) that would allow another to recognise a patient or someone close to them. In the new draft guidance on social media the only additional emphasis is on the impact of embedded information such as GPS co-ordinates that would allow us to know from where a tweet was made, or an image taken.
My own practice is that if I want to share a story about a patient that might allow them to recognise themselves then I ask permission, and I record that when sharing the story. So far this has only happened once and it was in a blog post. How could it be conveyed that a patient was aware and happy that their story was being shared on Twitter? If this is done in a separate tweet then those following the tweets may miss it and wonder if permission has been given. Is this something we need to be concerned about?
What about sharing images routinely made as part of care?
In 2011 the GMC gave additional guidance on the audio-visual recordings. For some images made as part of routine care, such as pathology slides, internal images of organs, and xrays, then no specific consent to take the images is needed. It is presumed that if the patient gives consent to the procedure then they give consent to the image being recorded. The guidances says that attempts should be made to make patients aware that they may be shared in an anonymised form, but there is no need to ask permission before doing this. This includes for publication in widely-accessible media such as press, print and internet. We can presume this includes Twitter!
The draft social media guidance makes no additional comment on this so sharing an anonymised image on Twitter for teaching purposes seems acceptable. But images are rarely of much value without an accompanying story. So we are back to the situation above. How much permission is it good practice to obtain before sharing a story? And we have to remember that the real-time nature of social media means that a story about a patient might be shared as it is happening, rather than six months later, so that it is more likely that people may recognise themselves or others.
Other images that are made as part of routine care, but are not part of a procedure, such as an image of the outside of the body, do need specific consent to be given. And again patients should be made aware that these images may be used for teaching or research, but specific consent does not have to be given for them to be shared for this purpose as long as they are anonymised and all identifying details are removed. However, the guidance states that if the image is to be shared in widely accessible media (eg Twitter or a blog) then if the image is identifiable consent must be obtained. If the image has been anonymised then good practice is that consent should also be obtained but," if it is not practicable to do so, you may publish the recording, bearing in mind that it may be difficult to ensure that all features of a recording that could identify the patient to any member of the public have been removed."
What about recording an image to share in an educational discussion on social media?
The GMC guidance which applies here is the section on "recordings for use in widely accessible public media". Here, even if the patient is not identifiable, and has been anonymised, consent must be given explicitly. Paragraph 37 states:
"You must get the patient's consent, which should usually be in writing, to make a recording that will be used in widely accessible public media, whether or not you consider the patient will be identifiable from the recording"
We are also obliged to check with our employers what their policies are. Some trusts prohibit the use of mobile phone cameras by staff to protect patient confidentiality.
If consent has been obtained from patients to share their non-identifiable images online, how can we share that information in a tweet? Can we presume that if we see an image shared on Twitter then the person sharing it has followed the correct policies, just as when we see an image in a journal we might presume that the correct policies have been followed? Should those leading case discussions develop their own policies and make these accessible from their Twitter profile?
Medical education on Twitter is fantastic. There are no professional or geopgraphic boundaries to discussions. And no boundaries to patients participating either! I want to see all that is happening already continue and also for more people to get involved. I think that by considering these issues and showing how we can be safe and transparent we can take these discussions to a new level of participation.